Improvement: FEATURE
Increasing geographic equity in access to kidney transplant
Kidney committee leaders discuss the path to new policies that put patients first.
Vincent Casingal, M.D., recalls experiencing his first transplant meeting more than 20 years ago. “What amazed me then and now was the collaboration of everyone involved working to improve patient care and wanting advancements in transplant.”
Casingal, a transplant surgeon and current chair of the OPTN Kidney Transplantation Committee, reflects that some of the big topics 20 years ago—things like increasing living liver donation and improving results in kidney donation—have seen major improvements in the past two decades, and he feels grateful to have been a part of the process.
This includes the recent changes to kidney and pancreas allocation, which are projected to increase equity in access to transplant for kidney and pancreas candidates across the country. Implemented March 15, the package of changes aims to distribute organs more fairly to people waiting for an organ, and has incorporated input from both patients and professionals. Fittingly, these patient-focused policies have launched in National Kidney Month, a time when communities across the country work to raise awareness about kidney disease.
More than 91,000 people in the U.S. are waiting for a lifesaving kidney transplant—patients waiting for them make up nearly 85 percent of all waiting list candidates in the nation. The new policies will help ensure that those candidates will have more equal opportunities to receive a transplant no matter where they live or are listed for a transplant, ensuring the right organ gets to the right patient at the right time.
The need for change
Before the new policies took effect earlier this month, the way a kidney (or a pancreas) was distributed meant:
- A kidney match would first be offered within its donation service area (DSA), the geographical area designated for organ recovery by organ procurement organizations (OPOs). There are currently 57 OPOs serving the U.S.
- If a kidney offer was not accepted within the DSA, the next phase of offers would extend to the administrative region in which it was recovered. There are 11 regions in the Organ Procurement and Transplantation Network.
DSAs and regions were never optimized for organ allocation, and the improvements implemented this month will help ensure that organ distribution is based on the medical needs of patients rather than artificial boundaries related to organ recovery.
Putting patients first
On March 15, 2021, the Organ Procurement and Transplantation Network implemented new circle-based policies for kidney and pancreas that complete the removal of the old system of organ allocation, which used 58 donation service areas of widely varying geographic size as units of distribution. Drawn for administrative reasons, these boundaries were not designed to optimize organ sharing for the sickest patients.
Leaving behind this arbitrary system establishes a consistent measure of distance between the donor hospital and the transplant hospital—and most importantly, puts patients first. Learn more about the changes.
Policy development: Growth and evolution
Casingal says DSA-based allocation worked for many years—“transplant was built on it”— but it was time for change.
A veteran of multiple OPTN committees and review boards, Casingal is chief of the division of abdominal transplant and surgical director of the kidney transplant program at Atrium Health in Charlotte, N.C. The drawback to the previous DSA-based allocation system was, he says, “that there wasn’t a great way to fairly share kidneys across those borders, which is what really needed to change about how organs are distributed.” Comparing the previous DSA-based system to waiting in one of several lines at a grocery store, he explains that a major problem was not being able to merge people into other lines if the line they were in got stuck.
Martha Pavlakis, M.D., the kidney committee’s vice-chair, agrees. “I think the best way to understand the problem with the hard boundaries of a DSA is to think about the history and realize that nobody would have designed the system like that if they were developing policy in a forward-looking manner.”
Policy is important to Pavlakis, a transplant nephrologist and the medical director of kidney and pancreas transplantation at Beth Israel Deaconess Medical Center in Boston, Mass., and associate professor of medicine at Harvard Medical School. Taking a historical approach to understanding policy development, Pavlakis describes the early days of transplant as often involving hyper-local relationships between transplant programs and histocompatibility labs and OPOs.
While those institutional relationships made it easier to collaborate at the time, they also led to a hardening of regional administrative units that acted as boundaries for distribution, which could lead to disparities as kidneys began to be allocated nationally.
“When you look at the history of these transplant relationships, you understand why now we’re having to build something that just makes more sense for patients,” Pavlakis says. The motivator for her to work to change the allocation policies was the geographic disparity. “It makes no sense that if you are on a wait list just over one DSA boundary, your wait time plummets.”
A line on a map could leave a sicker patient waiting longer
As an example of how DSA boundaries could create inequities in organ distribution, Casingal describes how a person who lived on one side of the Hudson River would likely wait significantly longer for an organ that someone living on the other side, even though they were very close in proximity. With the new policy changes, those disparities would flatten out with the elimination of the DSA boundary between them.
Casingal is eager to discuss broader access to kidneys: “I want everybody to have a kidney transplant. That’s my goal, and to set up a system that leads to that type of success.” Key to that success, Casingal feels, is supporting the work OPOs do to increase organ donation as well as working on the transplant side to increase organ offer acceptance rates and improve patient outcomes.
But he also stresses that the work is not done yet. “I think this is a big step—but not the final step toward reducing disparity in access.”
People waiting for a lifesaving kidney transplant
More than 91,000 in the U.S.—nearly 85 percent of all waiting list candidates in the nation.
The changes to kidney and pancreas allocation mean the first unit of distribution is now a 250 nautical mile circle drawn around the donor hospital. One of the primary goals of the fixed-circle policy is to grant kidney and pancreas candidates more equitable access to transplantation, regardless of where they live.
Statistical simulation modeling predicts the new policies will improve transplant access for key groups of candidates, including:
- Children
- Women
- Ethnic and racial minorities
- Candidates who highly sensitized and hard to match.
Read more about the changes.
Bringing patient perspectives into policy
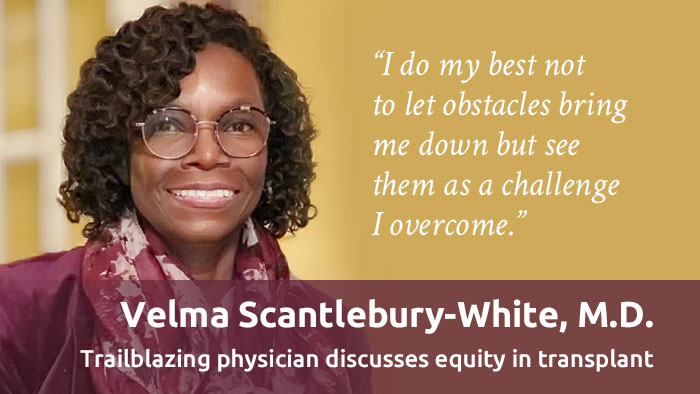
Policy is not solely in the hands of clinicians or other donation and transplant professionals. Patients and family members have a voice in how policy develops —and Pavlakis calls it a “gut-check” when a patient or family representative on a committee speaks up and makes their opinions known in committee meetings.
“Few of us as doctors are actually transplant patients,” she explains, observing that a patient representative is sometimes able to see things in a way clinicians can’t. “Patients and donors and patient and donor families can point out things they can see that we’re sometimes blind to. So that’s important. The clinical expertise on our side is crucial, but the balance of patient perspective is equally important.”
Casingal calls transplant a team sport—it begins with the patient and involves a range of donation and transplant processes every step of the way. So it makes sense to include a variety of perspectives and take a patient-centric approach to policy development. “You need people at every step of the way to give you their input,” he says. “If the goal is to improve allocation, then you have to get a diverse viewpoint of what’s happening now and how things can improve. Because it’s not one person or one viewpoint that will figure this out.”
Teamwork and shared values
When asked about the concern some may have about creating potential new disparities if transplants are reduced in one area and increased in another area, Pavlakis says that it comes down to shared values. “Resisting change means accepting that a candidate in one place waits eight years and another person in another place only waits two years.” Balancing advantages may impact some, she says, but “if people share the values that led to the change, then they can accept even some personal loss of advantage.”
But that brings her back to policy and the importance of participation—she advises all stakeholders to read and learn about the policies that lay out how organs are allocated, and come to the table with constructive input. “It all gets back to values—policy is the living, breathing expression of group values.”
What’s next in policy development?
Removal of DSA and region from organ distribution is not the end of improving organ allocation—it’s one part of a continuum of ongoing holistic policy development.
The donation and transplant community is working together on an allocation initiative called continuous distribution that can be adapted to all of the organ allocation systems.
Continuous distribution will make organ allocation more equitable because it means candidates will no longer be divided into rank-ordered classifications. Instead, all candidates will be considered at the same time and ranked with an overall score determined through a consideration of multiple patient factors. Pavlakis calls it “the most patient-focused way to allocate organs, because it’s about the patient rather than the transplant hospital or region.”
Learn more about the continuous distribution framework.
“It all gets back to values—and policy is the living, breathing expression of group values.”
Martha Pavlakis, M.D., Vice-Chair, OPTN Kidney Transplantation Committee