Living donation

In 2023, more than 6,900 people became living organ donors
Living donor supporters reached the summit of Mount Kilimanjaro on World Kidney Day, March 9, 2023.
Directed donation
Donating an organ to a family member or friend
Paired donation
Two or more pairs of living donors swapping to make a compatible match
Non-directed donation
Donating an organ without naming someone
On this page
Understanding living donation
How do I become a living donor?
Data on living donation
More resources
Understanding living donation
With living donation, a living person donates an organ or part of an organ for transplantation. Most living donors donate one of their kidneys or a part of their liver. Much more rarely, living donors may donate other organs. Living organ donors make thousands of transplants possible every year.
Relatives, loved ones, friends and even individuals who wish to remain anonymous often serve as living donors to spare a patient a long and uncertain wait. In 2023, more than 6,900 transplants were made possible by living donors.
If you are considering living donation, it is critical to gather as much information as you can from various sources.
Who can be a living donor?
Living donors should be:
- in good overall physical and mental health and
- older than 18 years of age.
Medical conditions such as uncontrolled high blood pressure, diabetes, cancer, certain infections, or an uncontrolled psychiatric condition, could prevent you from being a living donor.
Since some donor health conditions could harm a transplant recipient, it is important that you share all information about your physical and mental health. You must be fully informed of the known risks involved with donating and complete a full medical and psychosocial evaluation. Your decision to donate should be completely voluntary and free of pressure or guilt.
What are the types of living donor transplants?
The kidney is the most commonly transplanted organ from a living donor. One entire kidney is removed and transplanted. Living liver donation, where a segment of the donor’s liver is transplanted, occurs less often, and the donor is usually related to the recipient. Also, in rare cases, a uterus or segment of other organs can be transplanted from a living donor.
Directed donation
- a biological relative, such as a parent, brother, sister or adult child,
- a biologically unrelated person who has a personal or social connection with the transplant candidate, such as a spouse or significant other, a friend or a coworker, or
- a biologically unrelated person who has heard about the transplant candidate’s need.
If tests reveal that the donor would not be a good medical match, paired donation may be an option.
Paired donation
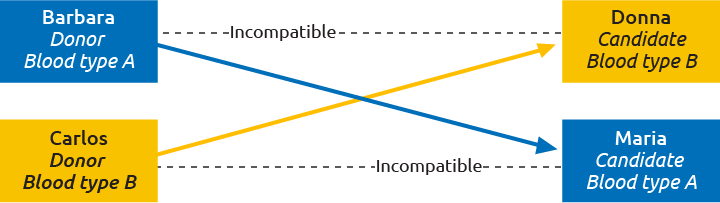
For example, in the diagram above, Barbara wants to donate a kidney to her sister Donna, but they do not have matching blood types. Carlos wants to donate a kidney to his wife Maria, but they are also not compatible. By “swapping” donors so that Carlos matches Donna and Barbara matches Maria, two kidney transplants are made possible. This type of exchange often involves multiple living donor/transplant candidate pairs.
Learn more
View participating transplant hospitals for the OPTN KPD pilot project.
Non-directed donation
Other donation types: blood type incompatible and positive crossmatch
Positive crossmatch donation involves a living donor and a transplant candidate who do not match because the candidate has certain antibodies (a protein substance) that will immediately react against the donor’s cells and cause the transplant to fail. Specialized medical treatment (plasmapheresis) is provided to prevent rejection. This type of donation is usually only considered when no other living donors match.
On this page
Understanding living donation
How do I become a living donor?
Data on living donation
More resources
Making a connection
How do I become a living donor?
Getting started
1. Contact a transplant hospital
If you know a person you would like to help through living directed donation, talk to him or her and contact the transplant program where the person is listed. If you would like to be a living non-directed donor, contact a transplant hospital of your choice to find out if they have this type of donation program. Visit the OPTN Member Directory for a complete list of transplant hospitals. When you contact transplant hospital staff, they will typically ask for your consent to begin a basic medical screening. With your consent, the transplant hospital staff will ask you questions about your medical history to find out if you have any conditions that would keep you from being a donor.
2. Have an initial screening
This initial screening is typically followed by a blood test to see if you are compatible with the intended transplant candidate. If you are not compatible with that person, you may have other options to donate. These options include paired exchange, blood type incompatible donation or positive crossmatch donation.
3. Get an independent donor advocate
Transplant hospitals are required to provide an independent donor advocate (IDA) or IDA team for all potential donors. Your IDA should not be part of the potential transplant recipient’s medical team. The IDA will assist you during the donation process.
Next steps
You will need to answer all the questions that are asked—this includes questions about behaviors that would place the recipient at increased risk of disease transmission. The transplant staff will ask about your financial situation and talk about who can give you physical help and emotional support throughout the donation process. You will be asked to fully describe your reasons for wanting to donate and how it might affect your lifestyle (such as employment and family relationships). Involving your loved ones in the educational part of the evaluation process can be helpful. They can learn about the donation surgery and recovery process and support you in your decision.
Tests
Psychosocial and/or psychological evaluation
This tool assesses your mental health; whether you feel pressure from others to donate; your ability to understand information and make an informed decision; and your daily life circumstances, such as the possible impact on your job, whether you would have any help while recovering from donation, and your family’s views about the donation.
Blood test
This is done to check blood type compatibility between you and the transplant candidate. It tests many things, including:
- Blood type compatibility
- Tissue typing: This blood test checks the tissue match between six codes on the transplant candidate’s and your white blood cells. The more matches that are found, the better the chance is that the transplant may be successful long-term.
- Crossmatching: This blood test determines how the transplant candidate will react to your organ. A “positive” crossmatch means that your organ will not match the candidate. A “negative” crossmatch means that your organ is compatible with the candidate.
- Blood tests to screen for transmissible diseases: These tests determine if you have HIV/AIDS, hepatitis, cancer, or other diseases. Some positive test results may need to be reported to local, state, or federal health authorities for public health reasons.
Urine testing
A 24-hour urine sample is collected to look at your kidney function.
Chest X-Ray and electrocardiogram (EKG)
These tests screen for heart and lung disease. Depending upon your age and medical history, other heart and lung tests may be needed.
Radiologic testing
These tests allow physicians to view the organ you want to donate, including its blood vessel supply. Tests can include a CAT scan, MRI, and arteriogram.
Gynecological examination
Female donors may need to receive a gynecological examination.
Cancer screening
Age and risk appropriate screening which may include a colonoscopy, prostate exam, mammogram, prostate exam, and skin cancer screening.
Questions?
Patients, family members, and friends needing additional information about living donation and organ transplant, contact the OPTN Patient Services Line at 1-888-894-6361 or [email protected].
Making an informed decision
The informed consent process should help you understand all aspects of the donation process, including the risks and benefits. This will include a discussion about alternative procedures or types of treatments that are available to the transplant candidate, including dialysis or transplant from a deceased donor. Your consent to become a donor is completely voluntary. You should never feel pressured to become a donor. You have the right to delay or stop the donation process at any time. The reasons behind your decision will be kept confidential.
Before making a final decision, talk with other people who have been living donors. Consider contacting your transplant hospital to learn more about what it’s like to be a living donor. Fully consider how donation may affect your physical and emotional health, as well as your family life, financial situation and current and future health and life insurance status. Talk in detail with your loved ones, such as family members and close friends.
Medical and psychological risks
Please note that there has been little national systematic long-term data collection on the long-term risks associated with living organ donation. Based upon limited information that is currently available, overall risks are considered to be low. Risks differ among donors and according to the type of organ you donate.
Possible long-term risks of kidney donation may include high blood pressure (hypertension); reduced kidney function, which may be measured by large amounts of protein in the urine; hernia; organ impairment or failure that may lead to the need for dialysis or transplantation; or even death.
Possible risks of liver donation include wound infections, hernia, abdominal bleeding, bile leakage, intestinal problems including blockages and tears, organ impairment or failure that could require additional treatments, surgery, or liver transplantation, or even death.
There may be other medical risks for each type of organ donation surgery, since there are limited data about long-term complications and since each donor’s surgery and recovery experience is unique.
Negative psychological symptoms are possible during the healing process and even years after the donation. Your donated organ may not function in the recipient after it is transplanted. You and/or the transplant recipient may have medical problems from the surgery. Scarring or other aspects of the donation process could contribute to problems with body image. You may have feelings of regret, resentment, or anger. You may have symptoms of anxiety or depression. Treatment for these conditions can be lengthy, costly, and could include the use of medications with risks and side effects. Ask your hospital for most up-to-date information available on the risks associated with living donation.
Recovery from surgery
As a kidney donor, you can generally expect to stay in the hospital for two days after surgery. Most kidney donors resume normal activities after four to six weeks, depending on the physical demands of their daily living and work tasks. You may not be able to drive for up to two weeks. You may have lifting restrictions for at least six weeks. Many donors have reported experiencing fatigue for varied periods of time.
As a liver donor, you may stay in the hospital up to a week, or longer in some cases. The liver typically regrows to normal size in two months. Most liver donors return to work and normal activities in two months, although some may need more time.
Every transplant hospital is required to report living donor follow-up data at six months, 12 months and 24 months post donation. Talk with the staff at the transplant hospital about their follow-up procedures. Ask for detailed information about follow-up office visits, laboratory tests, and other possible requirements, and who will pay for follow-up. Attend all follow-up appointments. What we learn about donor outcomes can help future potential living donors make informed decisions.
To consider
- Think about how the donation process may affect your daily activities.
- Who will serve as your caregiver and support you during your recovery, especially if you have to travel a long distance for the surgery?
- How much time off will you need from work?
- How will this affect your care giving responsibilities such as caring for a child or an elderly relative?
Positive aspects of living donation
A living donation makes it possible to schedule the transplant at a convenient time for the donor and recipient. Better genetic matches between living donors and candidates may decrease the risk of organ rejection. In addition, kidneys from living donors usually work immediately.
Many kidney donor operations are now done with laparoscopic surgery. This form of surgery is less invasive than other procedures and involves smaller incisions. As a result, it can help to minimize recovery time for the donor.
A living donor removes a candidate from the national transplant waiting list.
Financial and insurance factors to consider
The recipient’s insurance coverage usually does not include transportation, lodging, long distance phone calls, childcare, or lost wages. A living donor cannot be paid for the donation because it is illegal under the National Organ Transplant Act of 1984. However, living donors may receive reimbursement for certain expenses related to the donation process.
You should talk about any financial concerns with the transplant hospital social worker or financial coordinator. They may have resources available for you. The National Living Donor Assistance Center, www.livingdonorassistance.org or (703) 414-1600, may be able to provide financial help for travel, lodging, meals, and other non-medical expenses connected with your evaluation, surgery, and follow-up services (within 90 days after the donation).
Transplant hospitals must submit follow-up data to UNOS on living donors for two years after the donation surgery. It is important to ask your transplant team about payment for follow-up care. The hospital and the recipient’s insurance may not cover these costs.
Most kidney transplant candidates have Medicare, which may provide coverage for donors who have donation-related complications. For more information, contact Medicare by phone at 1-800-MEDICARE or at www.medicare.gov. Talk with your transplant hospital about medical and disability insurance that covers problems that may occur from the donation. Some hospitals may provide these policies free of charge, while others may offer them for purchase.
Some donors have reported difficulty in getting, affording, or keeping health, disability, or life insurance. It is important that you talk with your own insurance carrier before making a decision about being a living donor. Your premiums could increase. If you do not have health insurance, serving as a donor could be considered a pre-existing condition if you apply for insurance later.
If you work, talk with your employer about leave policies before committing to living donation. Also, think carefully about the financial impact on your family, especially if you and/or your caregiver during the donation recovery process may face lost wages.
Considering living donation
The process of making a decision
Directed liver donation

Data on living donation
Reviewing national and transplant hospital data may affect your decision to become a donor; however, there are limited long-term data available on how living donors do over time.
Since June 2006, UNOS has provided a patient safety system for transplant hospitals to report medical problems experienced by living donors for two years after the donation surgery. Although major adverse events are rare, hospitals must report to UNOS if any of the following events happen within two years of the donation surgery:
- living donor death
- loss of a function in a donor’s remaining kidney or other organ of which a portion was donated
- any organ that could not be transplanted or is not used for original planned recipient
Talk with your transplant hospital about their living donor follow-up procedures and ask about data they have collected. They are often able to provide you useful information such as:
- the number of living donor surgeries performed at the hospital,
- the percentage of living donors who receive two years of required follow-up,
- the number of living donors who have had medical problems, including any incidents reported to the UNOS patient safety system,
- transplant recipient and transplanted organ survival rates and
- any Medicare outcome requirements that the hospital has not met (such as meeting expectations relating to number of transplants done and recipient and organ survival rates).
See waiting list total and more transplant trends.

 Read more:
Read more: