Learn how:
- Candidates receive transplant priority based on their level of illness.
- Transplant candidate’s transplant hospital may seek an exception score.
- To appeal a decision to an application for an exception.
How do we ensure equity for all patients?
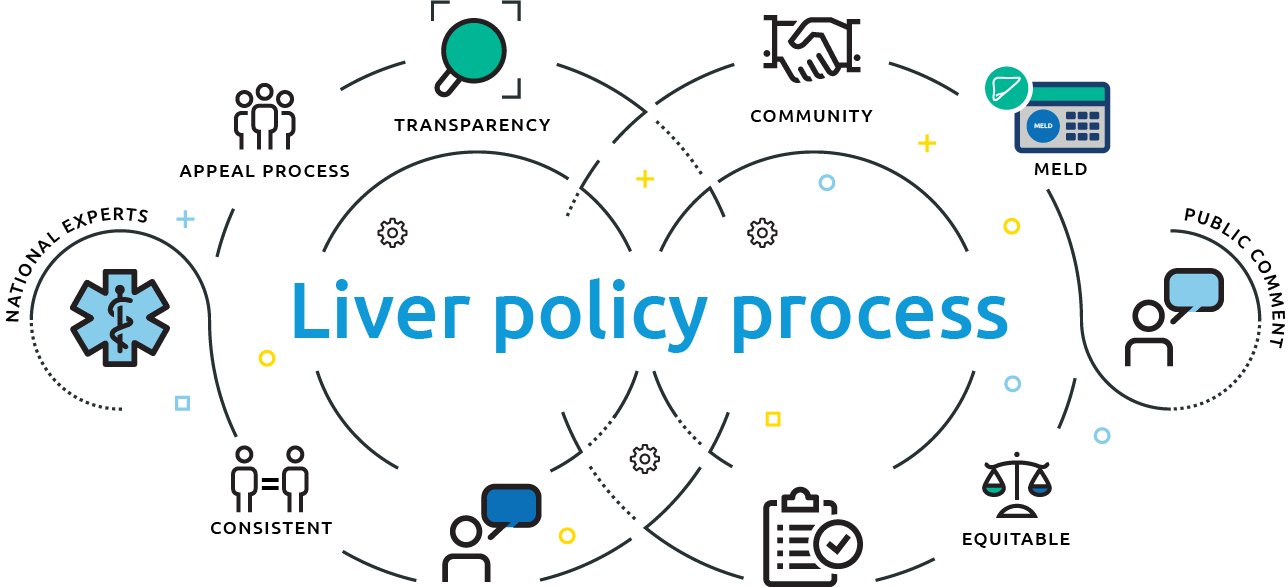
The national liver allocation system is designed to consider all transplant candidates in an equitable and consistent manner, understanding that there are currently not enough organs to transplant all in need. Liver allocation policy — the policy that matches deceased donor organs with patients on the waiting list — is developed with extensive input from the public and the community of donation and transplantation professionals.
Exception scores may be an option for liver transplant candidates whose medical circumstances require special attention. The following information explains how a candidate’s transplant hospital may seek an exception score and how it may appeal a decision regarding exception.

National Liver Review Board
How does it help patients?
Volunteer medical experts consider all exception requests on an anonymous basis, to ensure the system works fairly, objectively and consistently for all patients.
Our vision
Working together to make the national transplant system equitable for all
A message from Brian Shepard, CEO (former), United Network for Organ Sharing
UNOS is a mission-driven, nonprofit organization that brings together the donation and transplant community to establish a transplant system that is fair, objective and consistent for every patient on the waiting list.
Read the full letter here
Volunteers representing the transplant field are at the heart of what we do. In fact, we have many more volunteers than paid UNOS staff members, and those volunteers are transplant doctors, organ recovery teams, health care professionals, donor families and patients from all over the U.S. Our goal in bringing this community together is to do everything we can, every day, to improve the system and work to find patients the life-saving organs that they need.
How we develop policy
Because there aren’t enough organs to meet the need, as a community we develop policies that offer available organs in as fair a way as possible. Policies are developed by our volunteers who serve on committees focused on subject areas—liver transplantation or kidney transplantation, for example—and on committees that ensure equity in the system around particular perspectives, including patient affairs or minority affairs. Those committees develop proposals for ways to strengthen allocation policy.
Every policy proposal is available for public comment on our website. Twice each year, we hold a series of meetings around the country where the public can come and comment on those proposals. They are then voted on by a board of directors that is also elected from the national transplant community.
We welcome this productive exchange of ideas because it makes our policies better—and we think developing policies that are based on evidence and clinical practice is the best way we can serve the patients who rely on us to help them.
The process of assigning medical priority for liver transplant candidates
The primary way that candidates get ranked for a liver transplant is through a score that’s based on their lab values and other medical tests.
There is a process, however, that allows for a candidate who has a unique medical situation where the lab values don’t quite reflect exactly what their true medical condition is. In those cases, their transplant hospital can apply for an increase in the patient’s score based on those unique medical conditions.
That application is reviewed by a committee of liver transplant doctors from across the country who look at the patient’s condition and the additional information from the patient’s hospital and see if the score should be adjusted.
If that answer doesn’t satisfy the transplanting hospital, they can appeal that decision. And the appeal can include conversation where the transplant hospital gets to talk directly to the review committee and explain their case and answer questions the reviewers may have. The review board system was set up to be consistent and unbiased and to gather the information they think is most essential to support their decisions.
Improving the field of transplantation
UNOS is the one place where the donation and transplant community works together to address the organ shortage by finding new ways to utilize every possible organ that is donated.
We examine the data that we’ve collected through our years of managing the nation’s transplant system to look for any opportunity for improvement. We recently conducted a collaborative improvement project during which we worked with a number of transplant centers to find ways to identify and utilize hard-to-place kidneys, and we found that the number of these transplants increased overall.
Our vision
During each of the last seven years we’ve set a new high for the number of transplants. In 2021, we surpassed 40,000 people in the U.S. receiving transplants in a single year—a historic first for the nation. That number is thanks to the generosity of organ donors and their families, and we’re doing everything we can to honor the gift that they make.
Can we do more and better? Yes. We’re actively and continuously improving processes, both among staff and with the whole donation and transplant community.
A life-saving transplant for everyone in need—that is our vision. With the support of so many people who give the gift of life, and with the dedicated and talented people who work in this field, we are getting closer to realizing it.
A message to patients on the waiting list
MELD scores and PELD scores
For most liver transplant candidates, medical urgency is determined by an evidence-based formula, either MELD for candidates age 12 and older or PELD for those younger than 12. Each formula uses objective medical data to assess how likely a person is to survive in the short term without a liver transplant.
What is an exception score?
Some transplant candidates have a medical condition, such as cancer or rare forms of chronic liver disease, where MELD or PELD will not accurately predict their short-term transplant need. If so, they may qualify for an exception score — a separately assigned score to be used instead of their calculated MELD or PELD in matching the person for available organ offers.
The goal of exception scores is to make access to transplant more equitable among patients with similar levels of medical urgency.
Standard exception scores
Some medical conditions (for example, certain forms of liver cancer) are common enough that the liver transplant candidate can get a standard exception score – the same assigned score for any person with that condition. To qualify for a standard exception, the liver program needs to document that the person’s medical condition meets criteria outlined in OPTN policy.
For most medical conditions involving a standard exception, the candidate will get a score that is indexed at a level of urgency similar to people who don’t have exceptions. This index is based on a calculated score for each hospital where there could be a liver donor.
Median MELD at Transplant (MMaT) scores
For MELD patients (age 12 or older) with an exception score, the index that is used is based on the median (statistical midpoint) of MELD scores for people who recently have had liver transplants within an area surrounding the hospital where the individual liver donor is. This value is called the Median MELD at Transplant (MMaT).
The MMaT will be unique to each donor hospital, based on the scores of recently transplanted recipients in that area.
For example, at one donor hospital, half of the liver recipients transplanted nearby had a MELD score higher than 31, and half had a MELD score lower than 31. The midpoint of those scores – the MMaT – will be 31 for that donor hospital. The median differs from one hospital to the next.
At the time of a liver offer, most candidates with a standard MELD exception will have a score, for that individual offer, of three points less than the MMaT of that specific donor hospital. If the donor hospital has a median of 31, these exception candidates all will have a score of 28. For a different liver donor at a different donor hospital with a median of 29, the exception candidates will have a score of 26.
This approach is designed to ensure that exception candidates are compared the same way with each other, and that they have appropriate transplant priority for that liver offer alongside other non-exception candidates who have a score based on the MELD calculation.
Median PELD at Transplant (MPaT) scores
Liver candidates younger than age 12 may qualify for a standard exception that is based on the statistical median (midpoint) of transplants performed nationwide for children with a PELD score. This median score is known as the Median PELD at Transplant (MPaT). Unlike the median MELD, the MPaT is calculated based on all transplants done nationwide for children with a PELD score. Thus the MPaT is the same value for all candidates nationwide with a PELD exception, and it does not vary by the donor hospital.
Most transplant candidates with a standard PELD exception will have a score equal to the national median (MPaT) when being considered for organ offers. Again, this is meant to balance the transplant priority of PELD exception candidates in relation to one another and to non-exception candidates who have a PELD based their calculated score.
Customized exceptions and review of exception requests
Some candidates may be sicker than the standard exception score would indicate. In these cases, the person may have a condition that does not meet criteria for a standard exception score. In that instance, a patient’s transplant hospital (the transplant team) makes customized exception score requests to a national review board of independent medical experts made up of liver transplant physicians and surgeons.
In many cases, the custom score requested will again be indexed to the median MELD or PELD score at transplant (MMaT) or (MPaT), not a set score. This is done to balance the priority of a person with a custom exception score along with other transplant candidates, whether they have an exception score or not.
Requests examined by the review board contain no patient or hospital identifiers so that the review is completely unbiased and based only on medical information. The review board is tasked with deciding whether the requested score is reasonable based on the patient’s current medical condition and the likelihood that the recipient will do well once transplanted.
The National Liver Review Board
The National Liver Review Board (NLRB) consists of volunteer medical experts who practice transplantation throughout the United States. It considers all exception requests on an anonymous basis, with no information about the candidate’s identity or the hospital making the request. The board makes its decision based solely on the medical facts supplied by the transplant hospital, aided by their own medical judgment and guidance from the OPTN. The review board may grant or deny the exception score requested.
If the initial request is denied, the transplant hospital listing the candidate can choose to pursue a series of up to three appeals. Through the appeal process, the patient’s transplant team has the opportunity to provide additional detail to clarify questions that may arise in earlier review. In each instance, the reviews are conducted based on the medical facts presented, the medical expertise of the reviewers and applicable OPTN guidance.
“The NLRB provides a fair and consistent approach across the country for waitlisted patients whose need for liver transplant may not be adequately captured by their calculated MELD score.”
Julie Heimbach, M.D.
Mayo Clinic, Rochester, Minnesota
How the review board works
The National Liver Review Board (NLRB) was implemented in 2019. It replaced a system of 11 separate review boards, one for each OPTN Region.
The NLRB provides consistency by using national guidance to assess exception scoring requests. It consists of three specialty boards (adult hepatocellular carcinoma diagnosis (HCC); Pediatrics; and Adult Other Diagnoses). This ensures that needed expertise is present on each board and improves consistent decision-making. Each review board consists of members from across the country.
A number of medical conditions may qualify the candidate for a standard exception. This is a fixed value relative to the median MELD or PELD score for recipients recently transplanted in the area surrounding their transplant program, surrounding area at the time they received their transplant.
In other instances, the candidate has a condition that does not meet requirements for a standard exception. If so, the candidate’s transplant team provides medical information to the NLRB and requests a custom score they believe is appropriate.
The NLRB uses established guidance and medical judgment in deciding whether to grant or deny the hospital’s exception point request.
NLRB membership and process
Every liver transplant hospital can be represented on the NLRB. Each liver transplant hospital may appoint a representative and alternate to each of the specialty boards. Review board members are trained before they begin service on topics including exception policy, operational guidelines, and guidance for evaluating common types of exceptions.
For each exception request, the five assigned anonymous experts log into a secure web-based application, where the patient’s liver transplant hospital has posted both clinical data about the patient (identifiers removed) and narrative information in a free text field for reviewers to examine. The transplant hospital also requests the exception score it thinks appropriate.
NLRB members review each application to ensure that the score requested meets the clinical situation. Reviewers consider only medical information. They do not get information identifying the patient, the hospital, or the part of the country where the patient is waitlisted.
The review board members approve or decline the exception score requested. Reviewers vote on the site, and once two “No” votes or four “Yes” votes are received, voting closes. A request must achieve four of five affirmative votes in order to be approved. If an NLRB member votes to deny a request, he/she must provide an explanation.
Appeal process
If the NLRB declines a requested exception score, the transplant hospital may appeal the decision for further consideration. The first appeal goes back to the same panel of five reviewers that denied the request the first time. This gives the hospital a chance to provide more information and respond to any comments that the review panel provided.
If the initial review group declines the first appeal, the hospital can appeal to a different group of reviewers, called the Appeals Review Team (ART), which has nine members who meet weekly by conference call. The hospital requesting this second appeal has the opportunity to join the call, explain any nuances in the case, and have a two-way discussion with reviewers.
If the ART appeal is not favorable, the hospital may appeal to the OPTN Liver and Intestinal Transplantation Committee.
“Patients and their families rely on the transplant community to use the best medical judgment in every case and to be good stewards of the precious resources given us by donors and their families.”
David C. Mulligan, M.D., FACS
Yale-New Haven Health Transplantation Center
Past President, UNOS Board of Directors
Exception review & appeal process

Reports, news and FAQs
- Updated 12-month monitoring report available
- Findings from the first 12 weeks of operation of the NLRB
News items
- Oct. 7, 2021: Updated NLRB exception requirements effective
- Sept. 29, 2021: Updated Median MELD at Transplant scores take effect
- July 2021: National Liver Review Board guidance documents updated
- Policy notice on National Liver Board implementation
FAQs
- Frequently asked questions about the National Liver Review Board (NLRB) for candidates and caregivers
- Liver allocation questions and answers
Other
What is the OPTN?
UNOS holds the contract with the federal government to operate the Organ Procurement and Transplantation Network (OPTN). The OPTN exists to help create and shape organ sharing policies that make the best use of scarce donated organs. The process takes new technologies and advancements into account, so policies are continuously changing in order to save as many lives as possible.
The OPTN follows a collaborative development process for policies that govern the allocation, procurement and transportation of deceased organs. This process encourages participation by the public and all areas of the transplant community. It also promotes equity among patients waiting for organs and allows us to modify policy to reflect current science and medical practice.
