IMPROVEMENT: Feature
Increasing the use of high KDPI kidneys
Three-year collaborative improvement project drives results
What if?
What if hospitals could test improvements quickly and then share what they learn?
What if transplant professionals from across the country could be given a secure space to interact virtually and in real time?
What if UNOS members and stakeholders could work together to increase organ utilization and improve transplant program outcomes, processes and relationships?
A three-year collaborative improvement pilot project at UNOS explored these questions and more in relation to increasing the utilization of moderate-to-high KDPI kidneys.
The Collaborative Innovation and Improvement Network (COIIN)— begun in 2015 and directed by the Health Resources and Services Administration (HRSA) for the Organ Procurement and Transplantation Network (OPTN)—sought to increase the transplantation of marginal or high KDPI kidneys and explore new methods of quality monitoring.
How the project worked
Two cohorts comprising transplant centers from across the country took part, working closely with their organ procurement organizations throughout the improvement process. Cohort A went first with 19 transplant centers, followed by the larger Cohort B’s 39 centers.
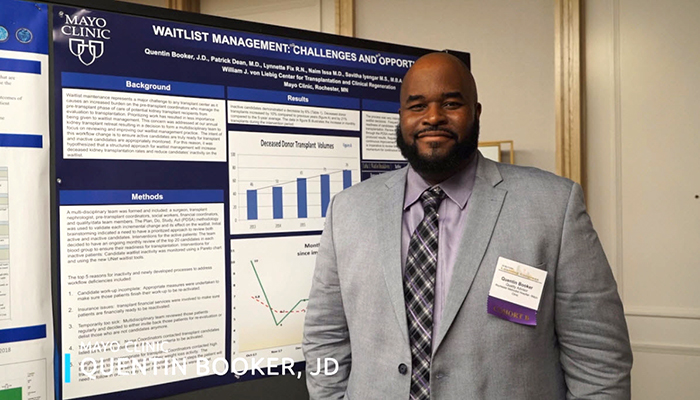
Each cohort worked within a nine-month timeframe of three 90-day improvement cycles related to the project’s key focus areas: waitlist management, organ offer and acceptance and care coordination.
Participating teams worked collaboratively with those of other centers and received on-site as well as virtual coaching from UNOS performance improvement specialists.
Rather than be prescriptive, centers were urged to develop and choose the tools that best fit their programs. A change that might deliver an improvement to a high-volume center with a longer waitlist such as Saint Barnabas Medical Center in northern New Jersey, may not have the same impact on a smaller-volume program with a different population, like Willis-Knighton Medical Center in Shreveport, Louisiana. Increasing communication between transplant staff and OPO staff in order to drive improvements might mean meeting monthly for a center like Seattle’s Virginia Mason and quarterly for others such as Piedmont Hospital in Atlanta.
The bottom line? No technique or tool could achieve universal success because every organization is different. What all of the participants shared however, was a desire to increase kidney transplantation overall—the waiting list for kidneys is longer than for any other organ. Working in a rapid-cycle of improvement and using a Plan-Do-Study-Act approach allowed centers to see changes happen quickly. The access to real-time data results meant improvement actions could be evaluated and adjusted as they were being implemented.
“We’re here to serve you as the OPTN to provide support, identify resources, build alliances, and to help our members get better. This COIIN collaborative is just the beginning.”
The result?
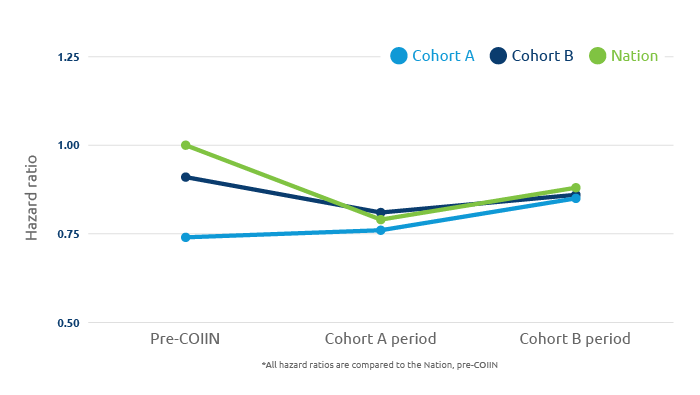
Data analysis of the project is still ongoing, but preliminary findings show an increase in the transplant rate and utilization of moderate-to-high KDPI kidneys was achieved in many participating centers. Early results also suggest that an approach that supports collaborative improvement in the transplant community can be effective at driving improvement.
To learn more about Cohort A’s results, read “Preliminary Findings from the First Pilot Phase of the Collaborative Innovation and Improvement Network,” published in the October 2018 issue of Transplantation. The paper was written by UNOS Assistant Director of Organizational Excellence Kristen N. Sisaithong, MA, UNOS Assistant Director of Research and Senior Research Scientist Robert J. Carrico, PhD, and Mayo Clinic Hospital Surgical Director, Kidney & Pancreas and UNOS Board of Directors member Kunam S. Reddy, MD.
Who participated?
Phase I/Cohort A
- Augusta University Medical Center, Augusta, GA
- Brigham and Women’s Hospital, Boston, MA
- Mayo Clinic (Phoenix), Phoenix, AZ
- Methodist Dallas Medical Center, Dallas, TX
- Northwestern Memorial Hospital, Chicago, IL
- New York-Presbyterian/Weill Cornell Medical Center, New York, NY
- Ochsner Foundation Hospital, New Orleans, LA
- Ohio State University Medical Center, Columbus, OH
- Oregon Health and Science University Hospital, Portland, OR
- Rush University Medical Center, Chicago, IL
- Scripps Green Hospital, La Jolla, CA
- Thomas Jefferson University Hospital, Philadelphia, PA
- University of Chicago Medical Center, Chicago, IL
- University of Colorado Hospital/Health Science Center, Aurora, CO
- University of Minnesota Medical Center, Minneapolis, MN
- University of Utah Medical Center, Salt Lake City, UT
- University of Virginia Health Sciences Center, Charlottesville, VA
- University of Washington Medical Center, Seattle, WA
- Virginia Mason Medical Center, Seattle, WA
Phase II/ Cohort B
- Banner University Medical Center, Phoenix, AZ
- Banner University Medical Center, Tucson, AZ
- California Pacific Medical Center, San Francisco, CA
- Cleveland Clinic Florida, Weston, FL
- Duke University Hospital, Durham, NC
- Erie County Medical Center, Buffalo, NY
- Florida Hospital Transplant Institute, Orlando, FL
- Hahnemann University Hospital, Philadelphia, PA
- Hartford Hospital, Hartford, CT
- Henry Ford Hospital, Detroit, MI
- Indiana University Health University Hospital, Indianapolis, IN
- Iowa Methodist Medical Center, Des Moines, IA
- Jewish Hospital, Louisville, KY
- Lehigh Valley Hospital, Allentown, PA
- Loyola University Medical Center, Maywood, IL
- Medical City Fort Worth, Fort Worth, TX
- Medical University of South Carolina, Charleston, SC
- Memorial Herrmann Hospital-Texas Medical Center, Houston, TX
- Mercy Health Saint Mary’s, Grand Rapids, MI
- Mount Sinai Medical Center, New York, NY
- Nebraska Medicine, Omaha, NE
- Piedmont Transplant Institute, Atlanta, GA
- Rochester Methodist Hospital-Mayo Clinic, Rochester, MN
- Sacred Heart Medical Center, Spokane, WA
- Saint Barnabas Medical Center, Livingston, NJ
- Saint Luke’s Hospital of Kansas City, Kansas City, MO
- SSM Health St. Louis University Hospital, St. Louis, MO
- St. Vincent Medical Center, Los Angeles, CA
- Strong Memorial Hospital/University of Rochester Medical Center, Rochester, NY
- Swedish Medical Center, Seattle, WA
- University Medical Center of Southern Nevada, Las Vegas, NV
- University of Alabama at Birmingham, Birmingham, AL
- University of California San Diego School of Medicine, San Diego, CA
- University of California San Francisco Medical Center, San Francisco, CA
- University of Iowa Hospital and Clinics, Iowa City, IA
- University of Kansas Hospital, Kansas City, KN
- University of Texas Medical Branch, Galveston, TX
- University of Texas Southwestern Medical Center, Dallas, TX
- Willis-Knighton Medical Center, Shreveport, LA