An ethical analysis examining the continuation of living donor transplantation during the COVID-19 pandemic
white paper
In this viewpoint, we consider how living donor transplantation fits within the priorities of a health system and whether its continuance is ethically justified during times of constrained resources.
Introduction
Living donor kidney and liver transplantation represents the optimal treatment for individuals with end-stage kidney and end-stage liver disease. These life-saving therapies are often contextualized as elective procedures based on the ethical principle of non-maleficence which correctly prioritizes protections of the living donor. These principles, guided decisions by many transplant hospitals to suspend living donor programs during the Spring 2020 surge of the Covid-19 pandemic. UNOS (United Network for Organ Sharing) has created an emergent topics program to address real-time ethical challenges with the aim of providing expedited guidance to the transplant community on critical issues. In this analysis, we explore the ethical issues regarding how living donor transplantation should be prioritized in times of healthcare scarcity, not to question past decisions which were made in unprecedented circumstances, but to develop an ethical framework to guide actions moving forward in an evolving environment that must balance several healthcare priorities.
Contingency vs. crisis standards of care
The emergence of the COVID-19 pandemic has required a dramatic and ongoing evaluation of how best to prioritize and distribute critical health resources in the setting of shortages. Immense demands of the staggering number of patients with COVID-19 continue to tax health systems, forcing them to transition to contingency standards of care and plan for crisis standards of care. Within contingency standards of care the spaces, staff, and supplies used are not consistent with daily practices but provide care that is functionally equivalent to usual patient care 1. Health systems sought to preserve functionally equivalent outcomes despite resource limitations by prioritizing surgical interventions where medical urgency largely drove immediacy of certain procedures while those deemed elective, such as living donor transplants, where delayed.
Setting priorities during times of critical resource scarcity is understandable and should be guided by ethical principles that include upholding the “rule of rescue,” maximizing benefit, safeguarding equitable access for the underserved, and promoting intrinsic and instrumental value 2 3. During the initial COVID-19 surge, many hospitals determined that living donor transplantation fell under the category of elective surgery, despite the fact that the Centers for Medicare and Medicaid Services (CMS) designate transplant procedures as tier 3b (high medical urgency) 4. Of course, the need to facilitate living donation to benefit both donor and recipient should be balanced against the risks associated with COVID-19 exposure during hospitalization, as well as considering institutional resource constraints facing hospitals in the midst of an active surge. This ethical analysis examines if proceeding with the living donor transplantation is appropriate when the goal is to provide contingency standards of care, and not crisis standards, as long as there are safeguards in place that minimize exposure risk, maintain staff expertise, and incorporate engagement of donor-recipient pairs in decisions about their willingness to accept the emerging and often unquantifiable risks of COVID-19.
Suspension of living kidney donation during COVID-19
In Spring 2020, the United States experienced the first surge of the COVID-19 pandemic. At that time, 81% of transplant centers in regions of the country with a high cumulative COVID-19 prevalence (>500 cases/100k population) chose to internally suspend their living donor kidney programs, although none formally inactivated their programs with UNOS 5. Transplant programs reported concerns regarding donor (85%) and recipient (75%) safety, as well as elective case restrictions (47%) as primary reasons for suspending living donor kidney cases 6.
Boyarsky et al. have analyzed data from the Scientific Registry of Transplant Recipients on the early effect of COVID-19 on kidney transplant outcomes. They show that new listings, deceased donor transplants, and living donor transplants declined by 18%, 24%, and 87%, respectively. Between March 15, 2020 and April 30, 2020, states with the highest rates of COVID-19 cases had the lowest rates of living kidney donor transplants (0.000.010.05), while these same States had a 2.2-fold higher observed waitlist mortality [1.882.222.62) 7.
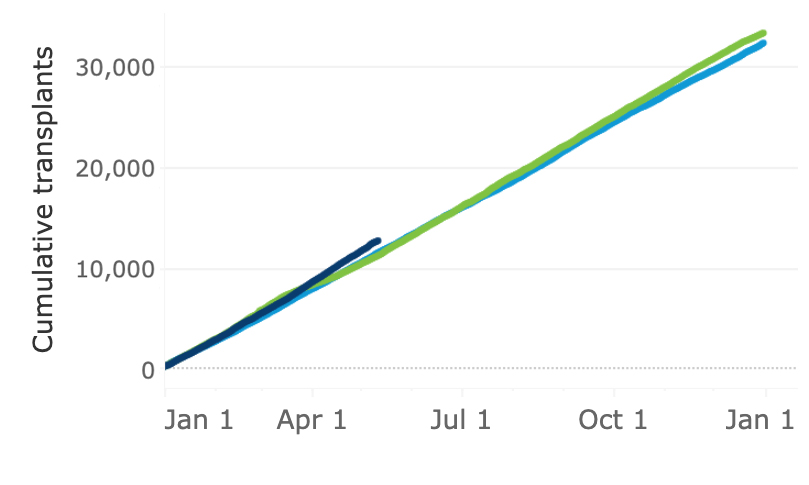
The first surge was associated with a decrease in total living donor kidney transplants performed compared to 2019, while the overall number of deceased donors was not impacted (Figure 1). This could represent the fact that the Spring 2020 surge was geographically limited, lending towards suspension of living donor transplant programs locally, while deceased donor grafts continued to be accepted in less affected regions. This is supported by the finding that deceased donor recoveries across organ types were reduced and disproportionately impacted the U.S. Northeast during the Spring 2020 surge 8. Currently, no analysis provides a causal association between suspension of living donor kidney programs and the observed rise in waitlist mortality. Additionally, it is also unknown how many approved donor-recipient pairs, whether scheduled for surgery or not, ultimately did not undergo living donor transplantation due to restrictions imposed by the COVID-19 surge and the impact of this on waitlist mortality.
Potential impact of COVID-19 on living donor liver programs
Although there was no appreciable difference between 2019 and 2020 in the number of living donor liver cases performed, subsequent surges of the ongoing COVID-19 pandemic may pose a threat to the volume of living liver donor cases as the pandemic progresses across the United States and engulfs more geographic regions. This only underscores the potential for an even larger number of patients and donors who might be forced to delay surgery or may be harmed due to a second wave of closures of living donor programs. Unlike patients with end-stage kidney disease who have the alternative of dialysis, patients with end-stage liver disease do not have a similar failsafe therapy to sustain them in the face of critical delays brought about by COVID-19 restrictions. Therefore, we posit that there are indeed harms to delaying living liver donor transplants because this subset of patients does not have options for sustaining survival other than transplantation and, as such, represent a patient population with a high level of medical urgency. In this context, we recognize that these decisions may be strongly influenced by transplant hospitals’ capacities, specifically blood product and ICU availability, that are necessary to perform liver transplants safely.
Ethical considerations: Intrinsic and instrumental value
In determining what priority to assign living donor transplantation, particularly in times of rationing, both intrinsic and instrumental value considerations become relevant. An intrinsic value refers to a normative preference that is inherently appreciated for its own sake, while an instrumental value is prudential, or strategic, and thus seeks to achieve a further end. The term instrumental value may have different applications in bioethics, but as used in times of rationing health care refers to prioritizing those – living donors – that have the means to save others 9. One’s health has intrinsic value for individuals in society-at-large; it is the principal and foundational goal on which all caregiving is predicated. In contrast, the manner in which healthcare ends are procured are often better understood instrumentally (i.e., with an eye towards calculating the strategic costs and benefits of the adopted approach).
The act of giving life through living donation has obvious intrinsic value, both for the recipient waiting for transplant, and for the living donor who is resolved to donate his or her organ for a recipient’s benefit. At the same time, there are instrumental values to consider in performing living donor transplantation in times of severe resource constraints, where the clear benefits to society of proceeding with a planned transplant must be balanced against critical resources being exigently distributed in other ways. In this case, there are a number of instrumental values to consider. For example, does our allocation of resources appropriately balance the interests of patients of specific disease state, like transplantation, with the needs of the population-at-large? Additionally, what is the impact of prioritizing one group in times of crisis and what are the potential longer-term effects on public perception in a manner in which it would negatively or positively impact donation rates? In considering the prioritization of living donation in such circumstances, the pragmatism of preserving existing relationships between health care providers must also be instrumentally evaluated, for example, between dialysis centers and transplantation centers. There are different levels of scarcity, capacity, and expertise that need to be considered and which are likely to be fluid. For example, a living donor recipient who is predicted to require an ICU bed may or may not be an appropriate candidate dependent on several health system factors that could change in a short amount of time.
Ideally, we would aim to pursue a policy where intrinsic values are reconciled with what we understand to be the greater good, and where instrumental considerations align and reinforce intrinsic goals. In considering how intrinsic values cohere with instrumental values, during times of crisis, it may be useful to identify critical thresholds beyond which we revisit standing policies in order to make sure that all of the relevant considerations are being taken into account.
Considerations of donor and recipient autonomy
The rationing of healthcare in times of resource scarcity is both required and ethical 10. These rationing decisions are determined by leaders of healthcare institutions who are aware of an institution’s level of resources and capacity. The intention is to balance maximal benefit with equality and instrumental value considerations. However, this calculus is not clear where the risk/benefit balance is uncertain. The ethical principles that govern organ transplantation are to balance considerations of utility, justice (equity), and respect for persons (autonomy) 11. While the tension between utility and justice is arguably heightened in times of severe health resource scarcity, autonomy considerations should have greater emphasis when the risks are not quantifiable, yet the benefits are well-established 12 13. During the Spring 2020 suspension of living donor transplantation due to the COVID-19 surge, transplant professionals pointed to safety considerations for both the donor and recipient as a primary driver for their decision to delay transplantation 14. For donors in particular, safety considerations are of paramount concern for transplant teams. However, as the exposure and outcome risks are ambiguous and dependent on several factors, including the local density of infections, engaging donor-recipient pairs in discussions regarding their perspectives of accepting risk promotes autonomy, enhances patient-centered care, and should have greater emphasis on clinical care decisions 15 16. In the context of comprehensive informed consent including shared decision-making, the UNOS Ethics Committee recommends that there is room for discretionary continuation of living donor transplantation in order to best serve the interests of liver and kidney patients, the transplant community, and to promote donor-recipient autonomy.
Recommendations for transplant community
These recommendations apply to transplants hospitals experiencing contingent standards of care and may not be applicable in conditions guided by crisis standard of care.
- Living donor transplants represent an important option for individuals with end-stage liver and kidney disease and should not be suspended uniformly when the aim is to provide contingency standards of care. Decisions to delay living donation may be appropriate given local conditions. However, these decisions should have on-going evaluation, be communicated transparently, and include timely dialogue with patients.
- Potential exposure risk to SARS-CoV-2 should not be the primary reason to delay living donor transplants, because the exposure and outcome risks are currently not quantifiable. Donors and recipients should be engaged in the process of documented shared decision-making, in order to understand their perceptions of what constitutes risk, as well as to come to a mutual appreciation of the social context which informs the willingness to undertake these risks.
- Transplant hospitals should strive to maintain a critical transplant workforce in order to avoid diverting this unique expertise in a manner which could negatively impact patient preparedness for transplant.
- As the understanding of COVID-19 outcomes in immunosuppressed patients continues to evolve, transplant hospitals should consider supporting protocols to ensure early detection of SARS-CoV-2 infections and include these measures as a discussion with patients during the process of shared decision-making.
Conclusion
Many transplant hospitals designate living donor transplantation as an elective procedure which makes these operations susceptible to temporary suspensions in favor of procedures categorized as emergent or urgent. Although CMS designates transplantation at a higher level of medical urgency (tier 3b), the elective nature of living donor transplantation reflects the general agreement that a living donor who undergoes surgery mainly to benefit others does so without pressure or urgency. It is understandable that under crisis standards, living donor transplant procedures should be delayed in favor of allocating crucial resources to the population-at-large. Given the uncertainty surrounding the risks and outcomes associated with hospital exposure to SARS-CoV-2, the UNOS Ethics Committee recommends engaging donor-recipient pairs in a process of shared decision-making and advocates for continuance of these procedures under contingency standards of care and within a framework of comprehensive informed consent.
Figure legend
FIGURE 1. Number of living donor and deceased donor transplants in 2019 and 2020 (to date). Adopted from unos.org/covid/ (accessed May 13, 2021).
2019
2020
2021
Living donor transplants
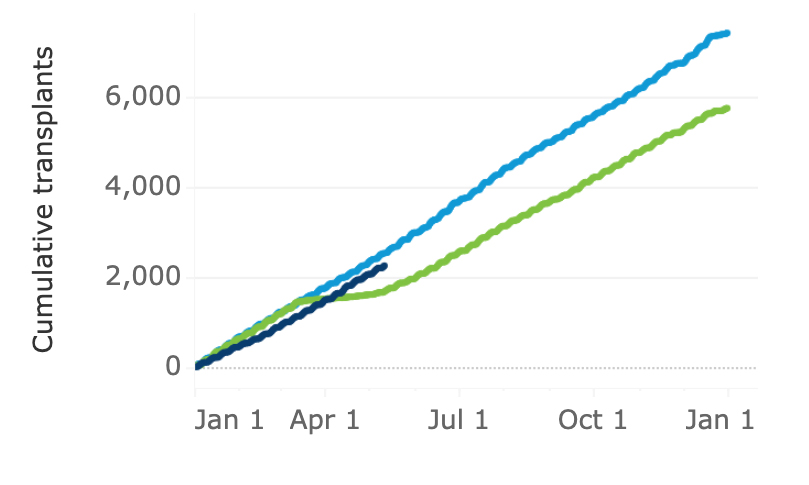
Deceased donor transplants
References
- Committee on Guidance for Establishing Crisis Standards of Care for Use in Disaster S, Institute of M. In. Crisis Standards of Care: A Systems Framework for Catastrophic Disaster Response. Washington (DC): National Academies Press (US). Copyright 2012 by the National Academy of Sciences. All rights reserved., 2012.
- Wall AE, Pruett T, Stock P, Testa G. Coronavirus disease 2019: Utilizing an ethical framework for rationing absolutely scarce health-care resources in transplant allocation decisions. Am J Transplant 2020;20(9):2332-2336.
- Persad G, Wertheimer A, Emanuel EJ. Principles for allocation of scarce medical interventions. Lancet 2009;373(9661):423-431.
- Services CfMaM. CMS Adult Elective Surgery and Procedures Recommendations. April 7, 2020. [cited 2020 December 14]; Available from: https://www.cms.gov/files/document/covid-elective-surgery-recommendations.pdf
- Lentine KL, Vest LS, Schnitzler MA, Mannon RB, Kumar V, Doshi MD et al. Survey of US Living Kidney Donation and Transplantation Practices in the COVID-19 Era. Kidney Int Rep 2020;5(11):1894-1905.
- Lentine KL, Vest LS, Schnitzler MA, Mannon RB, Kumar V, Doshi MD et al. Survey of US Living Kidney Donation and Transplantation Practices in the COVID-19 Era. Kidney Int Rep 2020;5(11):1894-1905.
- Boyarsky BJ, Werbel WA, Durand CM, Avery RK, Jackson KR, Kernodle AB et al. Early national and center-level changes to kidney transplantation in the United States during the COVID-19 epidemic. Am J Transplant 2020;20(11):3131-3139.
- Goff RR, Wilk AR, Toll AE, McBride MA, Klassen DK. Navigating the COVID-19 pandemic: Initial impacts and responses of the Organ Procurement and Transplantation Network in the United States. Am J Transplant 2020.
- Bernat JL. Ethical Justifications for Pandemic Rationing Strategies. In. Ann Neurol, 2020: 433-435.
- Scheunemann LP, White DB. The ethics and reality of rationing in medicine. Chest 2011;140(6):1625-1632.
- Organ Procurement and Transplantation Network. Policy 14: Living donation. 2014; Available from: https://optn.transplant.hrsa.gov/media/eavh5bf3/optn_policies.pdf
- Légaré F, Witteman HO. Shared decision making: examining key elements and barriers to adoption into routine clinical practice. Health Aff (Millwood) 2013;32(2):276-284.
- Politi MC, Lewis CL, Frosch DL. Supporting shared decisions when clinical evidence is low. Med Care Res Rev 2013;70(1 Suppl):113s-128s.
- Lentine KL, Vest LS, Schnitzler MA, Mannon RB, Kumar V, Doshi MD et al. Survey of US Living Kidney Donation and Transplantation Practices in the COVID-19 Era. Kidney Int Rep 2020;5(11):1894-1905.
- Institute of Medicine. Crossing the quality chasm: A new health system for the 21st century. Washington, D.C.: National Academy Press, 2001.
- Thiessen C, Gordon EJ, Reese PP, Kulkarni S. Development of a Donor-Centered Approach to Risk Assessment: Rebalancing Nonmaleficence and Autonomy. Am J Transplant 2015;15(9):2314-2323.
