in focus
Deceased donors with a history of COVID-19 are currently PCR-tested before organs are recovered.
In the third international town hall webinar, University of Pittsburgh Medical Center’s Fernanda P. Silveira, M.D., discussed potential risks associated with PCR positive and PCR negative donors and explained that continuing to gather more data will be crucial as the pandemic continues.
Transplant organizations from around the world continued their partnership to produce a third COVID-19-focused educational webinar for the international organ donation and transplantation community on May 11. During the webinar, health care professionals shared experiences to date and discussed how to prepare for the future of transplantation while the pandemic continues.
Panel topics included donor testing, how to emerge from quarantine, surgical prioritization, and the impact of COVID-19 on donor and transplant numbers.
Lewis Teperman, M.D., director of transplantation at Northwell Health, moderated a panel titled “What have we learned to prepare for the next wave?” During the panel session, Silveira, an infectious disease specialist, presented her talk, “Donors with history of COVID-19.”
Currently, deceased donors with a history of COVID-19 are tested with polymerase chain reaction, or PCR, which is a way to analyze a short sequence of DNA in very small sample.
Silveira discussed how she divides donors with a history of COVID-19 into two subgroups based on PCR results: Those with positive PCR at time of donation, and those with negative PCR at time of donation.
If a donor has positive PCR at time of donation, Silveira said the donor’s organs should not be transplanted due to:
- Risk of transmission to recovery teams and health care personnel.
- Risk of nosocomial infection, or hospital-acquired transmission.
- Potential risk to the transplant recipient. While donor-derived infection in transplant recipients has not been reported, it is conceivable.
If a donor has negative PCR at time of donation, Silveira outlined the following concerns:
- The graft quality of the donated organs will likely depend on any dysfunction suffered during the episode of COVID-19 (and possibly on the length of time since the illness).
- Those donors who required mechanical ventilation will present greater risk.
- Time from illness is an important factor—viral shedding can be prolonged, and the presence of the virus in donated organs is unknown. The longer the time since infection, the better the outcome for the recipient.
- Lungs and hearts carry the highest risk, while liver and kidneys likely carry less risk of graft failure.
Silveira stressed that because the presence of the virus in donated organs is not understood, continuing to gather more information will help shape the future of transplant in a time of COVID-19. As more of these donors and their organs become available it will be crucial to monitor graft and patient survival data, and to adjust decisions based on that data, she said.
Find the full recording of “COVID-19: Organ donation and transplant town hall international webinar #3” on UNOS’ webinar archive page.
In focus
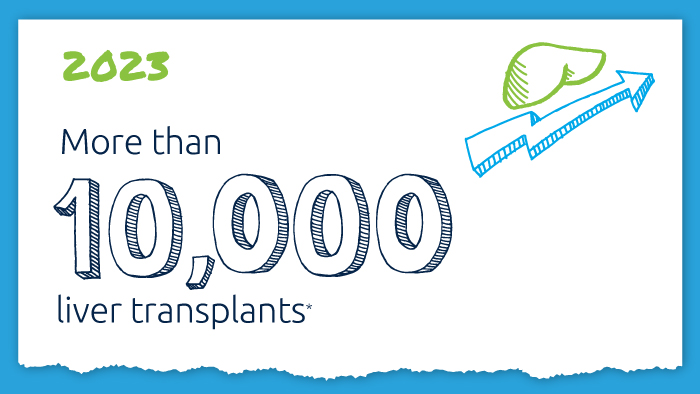
A decade of record increases in liver transplant
10,660 liver transplants, the most ever in a year.
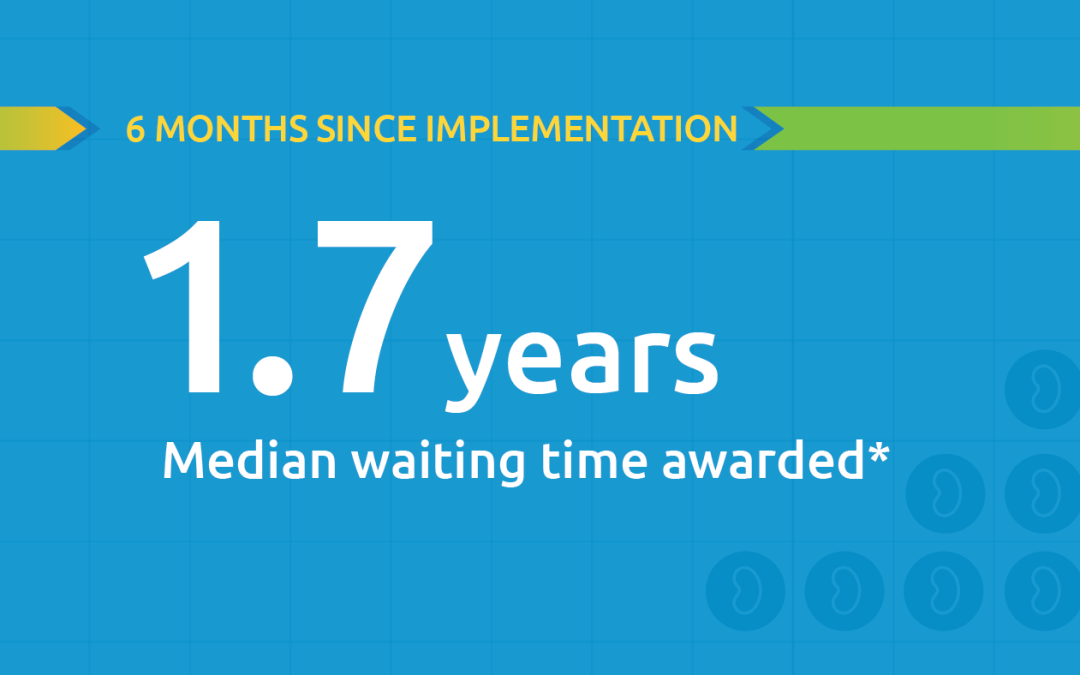
Black kidney candidates are receiving waiting time modifications, helping them get the organs they need
Latest kidney monitoring report shows two new kidney polices are working as intended

Research in focus: examining organ offers
Three recent studies from UNOS researchers examine offer acceptance practices and impact of Offer Filters tool.
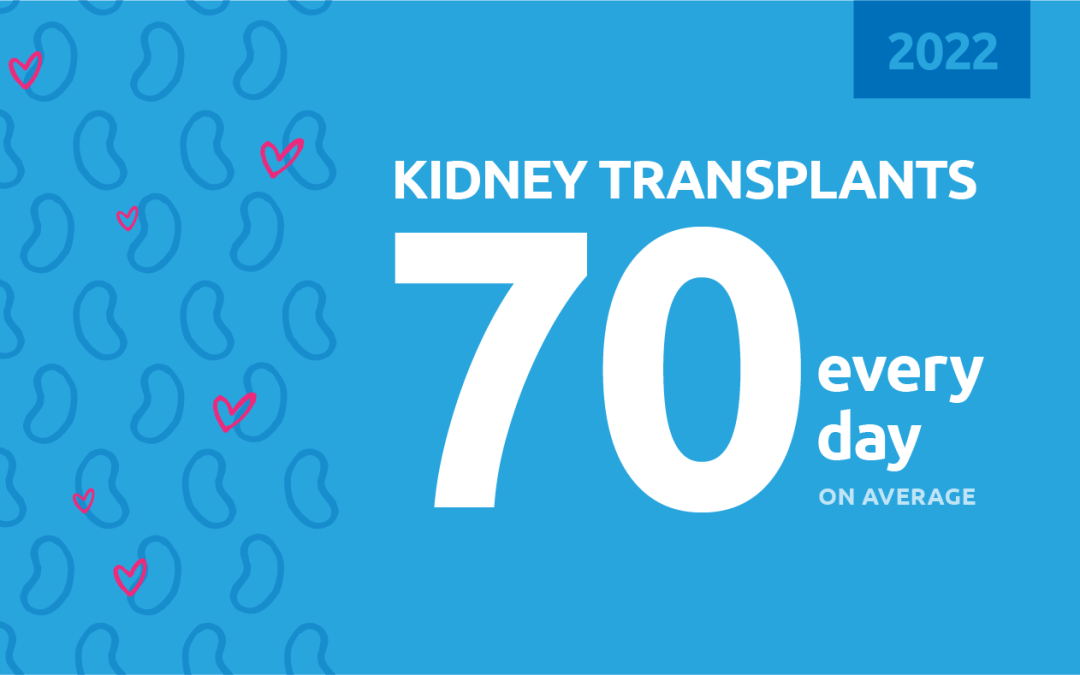
New milestone reached in kidney donation and transplant
For the first time, more than 25,000 kidney transplants were performed in a single year