in focus
Data reveals patient-centric policies allowed much-needed flexibility during a time of crisis.
Analyzing the impact of transplant policy and system modifications in response to the COVID-19 pandemic.
- Maintaining candidate allocation priority if a patient is unable to access clinical testing due to the pandemic.
- Relaxing data submission requirements.
- Incorporating donor COVID-19 infectious disease testing.
- Adding new COVID-19-specific offer refusal and candidate and recipient cause of death codes.
Researchers from United Network for Organ Sharing have analyzed these changes to determine their effectiveness in reducing burden, and recently presented their findings at the 2021 American Transplant Congress. The UNOS research team included assistant director of research Amber Wilk, transplant service line leader Sarah Taranto, associate policy analyst Courtney Jett and research science manager Laura Cartwright. Their project involved examining weekly OPTN data about candidates, donors, and recipients from March through April 2021.
“These were patient-centric policies designed to allow additional flexibility in a time of crisis,” explains Jett. “These policies required close monitoring to ensure they were meeting the needs of the patient population.”
The data findings revealed that through April 5, 2021:
- There was a continued decline in the percent of matches with at least one COVID-19 refusal reason for all organs.
- Kidney candidates had the highest proportion of COVID-19-related waiting list deaths among all reported deaths.
- All but one US OPO had 100 percent COVID-19 testing indicated in DonorNet® (via data fields, donor highlight text field, or attachment).
- UNOS’ data quality team has been able to confirm testing from all US OPOs and that all transplant programs were aware of testing results prior to transplant in instances in which testing was not reported in DonorNet.
“The data reflects the community’s continued commitment to provide the best care to their patients” says Wilk. “We saw an initial high usage of the policies that tapered as the community adapted and we learned more about the infectious disease. We also saw another uptick in usage around the holidays at the end of 2020 when the case counts began increasing again nationwide.”
The data also showed growth in the number and percentage of transplant recipient follow-up (TRF) and living donor follow-up (LDF) forms in amnesty status at the form’s due date since policy implementation, although variation was observed across OPTN regions and organ types. However, more recent data show a sharp shift. “Due to the herculean effort and diligence of transplant hospitals across the country, less than one percent of those forms are still expected, allowing the use of these data for both the normal policy development efforts of the OPTN and research into the impact of the pandemic on a national basis,” says Taranto.
The OPTN Executive Committee has been closely monitoring the status of both the impact of the pandemic and the use of the COVID-19 policies. While the addition of COVID-19 test results, refusal codes, and cause of death are permanent, several policies have since been deemed no longer necessary to support the transplant process during the COVID-19 pandemic.
“As centers adjusted their practice and the pandemic numbers stabilized, especially after vaccines were made widely available, the committee was able to sunset several of the policies,” says Cartwright.
Find all COVID-19 policy updates here.
There continues to be remarkable transplant community involvement in responding to the evolving challenges faced by the nation’s healthcare system. The U.S. has the highest-performing organ donation and transplant system in the world, even in the midst of a global pandemic. Despite a 50 percent drop in deceased donor transplantation early in the pandemic, the U.S. system recovered quickly and continues to outperform itself.
Wilk A, Taranto S, Jett C, Cartwright L. Summary of the OPTN’s Policy and System Modifications in Response to the COVID-19 Pandemic [abstract]. Am J Transplant. 2021; 21 (suppl 3).
Amber Wilk, UNOS assistant director of research
Sarah Taranto, UNOS transplant service line leader
Courtney Jett, UNOS associate policy analyst
Laura Cartwright, UNOS research science manager
Read more
In focus
A decade of record increases in liver transplant
10,660 liver transplants, the most ever in a year.
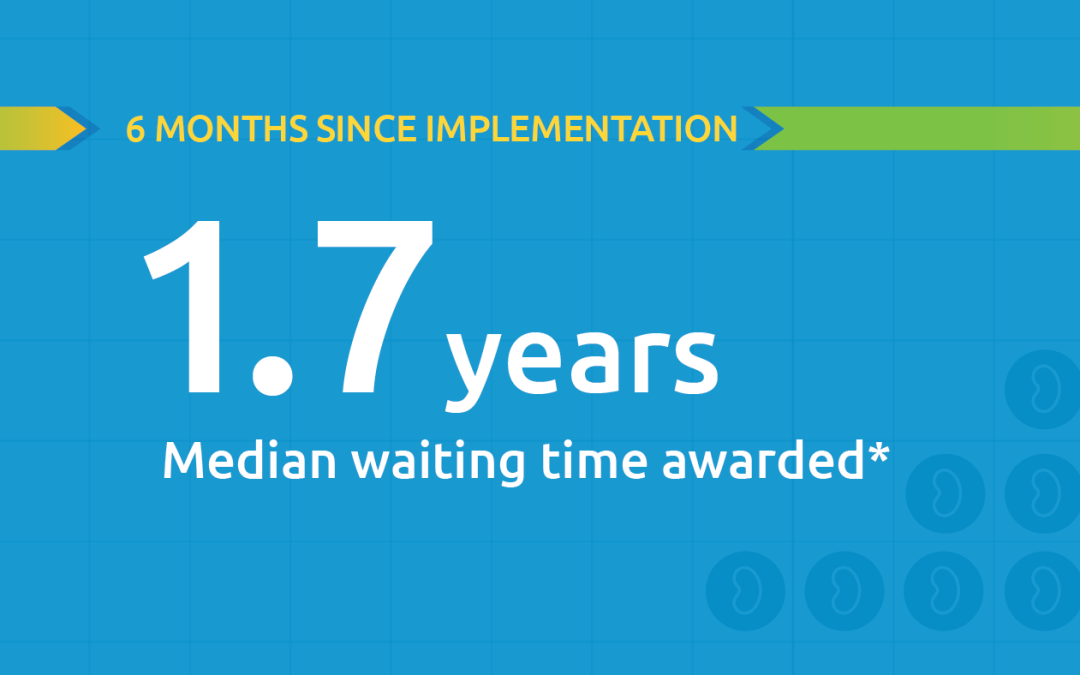
Black kidney candidates are receiving waiting time modifications, helping them get the organs they need
Latest kidney monitoring report shows two new kidney polices are working as intended

Research in focus: examining organ offers
Three recent studies from UNOS researchers examine offer acceptance practices and impact of Offer Filters tool.
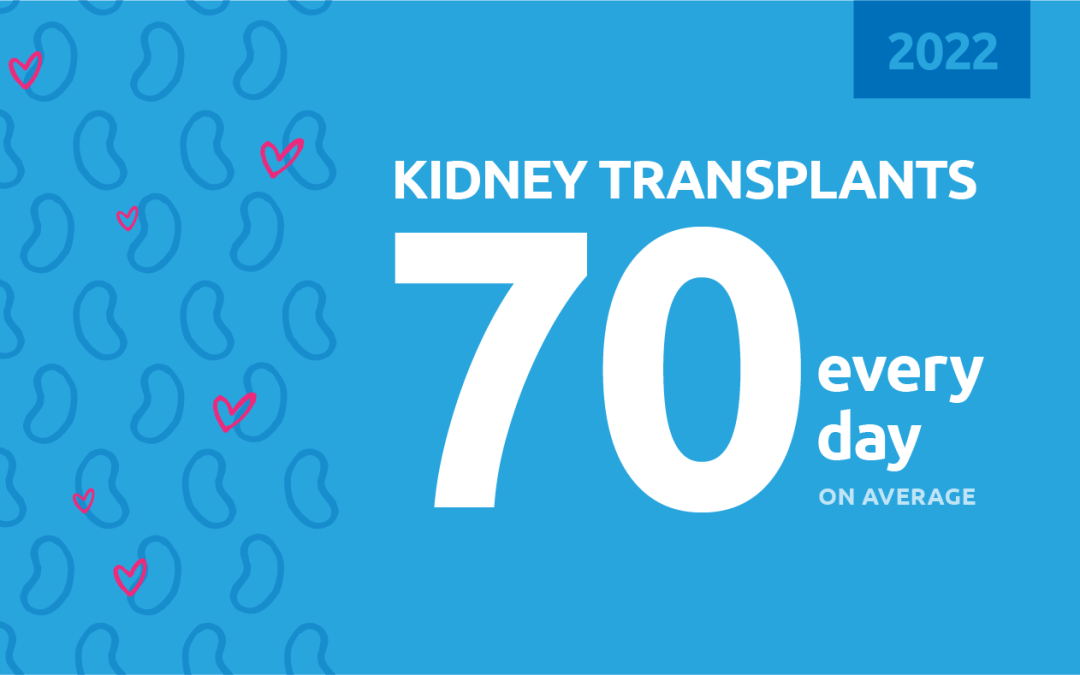
New milestone reached in kidney donation and transplant
For the first time, more than 25,000 kidney transplants were performed in a single year