INSIGHTS
Increasing lung utilization through organ perfusion
A transplant surgeon’s perspective on ex vivo organ perfusion
Matthew Hartwig, M.D., associate professor of surgery in the Division of Cardiovascular and Thoracic Surgery at Duke University Medical School, shares his experiences with ex vivo lung perfusion (EVLP) and the potential he sees in the technology.
Q. What EVLP technologies have been used in the Duke lung transplant program?
A. We have used the XVIVO XPS system, the TransMedics OCS for lung, and we are participating in the Lung Bioengineering clinical trial of a remote donor-lung perfusion facility.
Q. How has EVLP technology been used at Duke?
A. Until very recently the only way to use these devices was in clinical trials, so the main way we have been using all the devices is as a way to gather additional information about the organ prior to using it for clinical transplant. Also, one of the systems, the OCS, was recently approved by the Food and Drug Administration for use as an alternative storage technique other than the standard cold storage that we have done for decades.
Q. What is the benefit of that additional information?
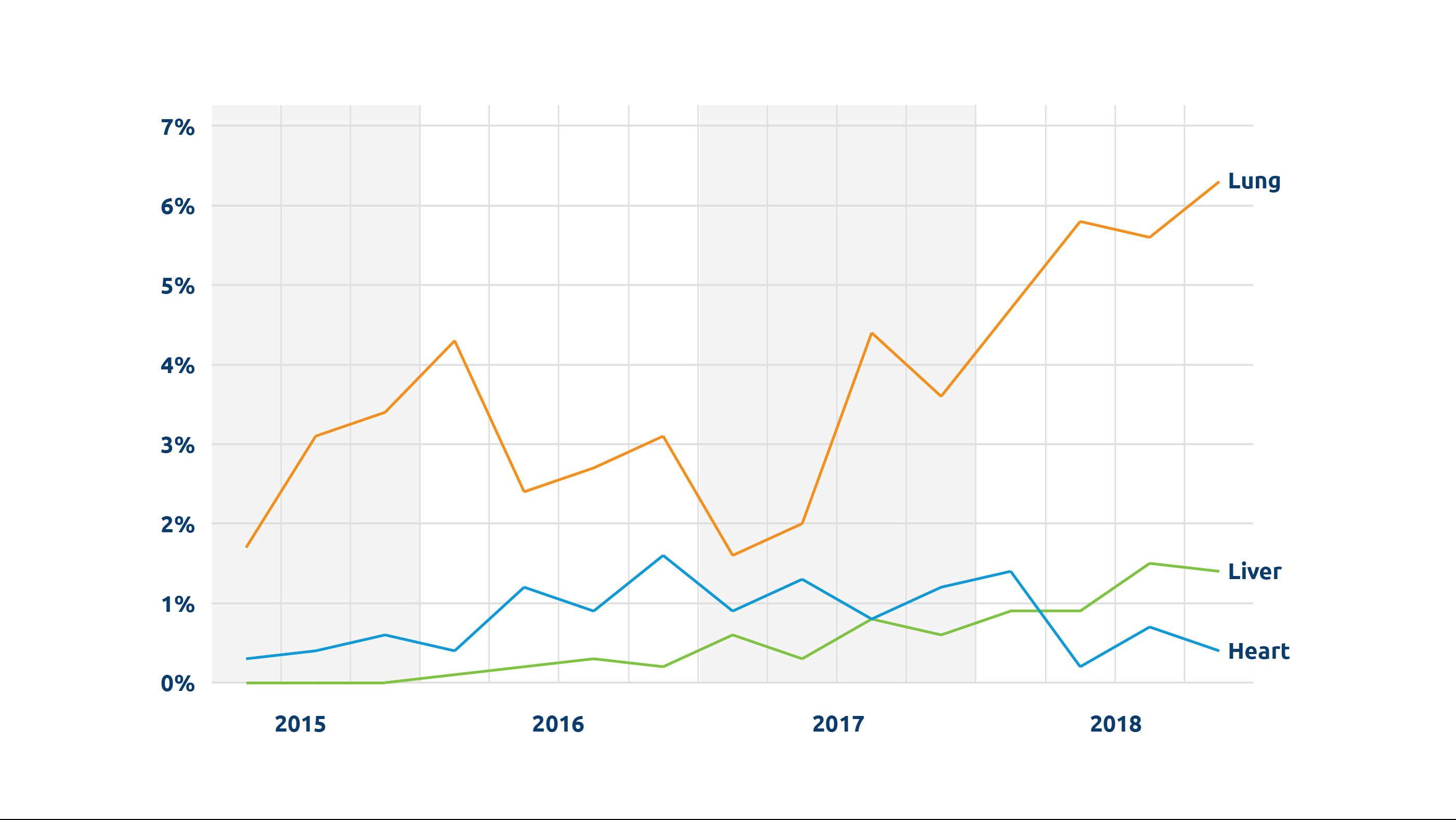
A. Lungs have the lowest utilization rate of any of the usual solid organs that are transplanted, and what is challenging is being able to accurately assess how well the organ functions and what kind of shape it is in when it has not yet been recovered from the donor. So these devices allow us in a very safe and reproducible fashion to assess the lung and evaluate its function in isolation, outside the complex environment of the donor. If the organ is on the device and working well, that seems to be a good signal for a positive outcome for transplant. We have been able to safely utilize some lungs for transplant that previously would not have been used because we didn’t have that information.
Q. What promise do you see for the future potential of this technology?
A. Although questions remain to be answered, ultimately this could be a better way to preserve organs than on ice. In addition, there is the potential that you could take lungs that are not currently usable, whether because of injury or infection or some other problem, and rehabilitate them. The next question is could we actually make a lung better for transplant—improve the function and enhance its long-term success? For example, you can even imagine being able to modify the lung in order to protect it from the recipient’s immune system. This may allow us to decrease the need for medications to prevent rejection long-term.
Q. What questions still need to be answered about EVLP?
A. No one really knows right now what is going to be the optimal way to use this technology. We still have a lot of work to do as a community to determine what is going to be the best way to perfuse, evaluate, rehabilitate and eventually improve the organ in an ex vivo setting.
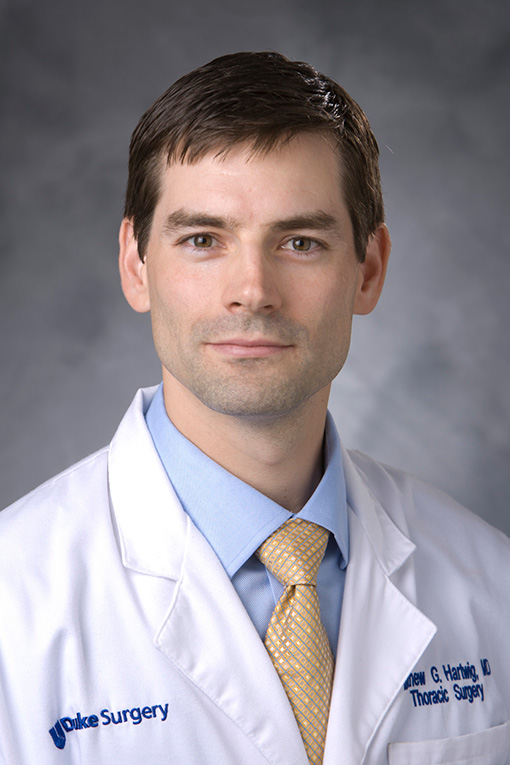
Matthew Hartwig, M.D.