INSIGHTS
The technology that could make more organs available
UNOS Chief Medical Officer David Klassen, M.D., discusses normothermic ex vivo organ perfusion and its potential to help save lives

David Klassen, M.D., UNOS Chief Medical Officer
Q. How is ex vivo organ perfusion currently being used in the U.S.?
A. In terms of establishing both the safety and immediate potential benefit of this technology, research is most advanced regarding the use of normothermic ex vivo organ perfusion to assess the function of individual organs. In the past, transplant surgeons really had to make a judgement about the acceptability of organs at the time of the procurement, but if you put them on the perfusion machine you can assess the function. If we can actively assess these organs, potentially we can increase the number of marginal or extended criteria donor organs—particularly lungs—accepted for transplant.
Q. How widely is the technology being used in the U.S.?
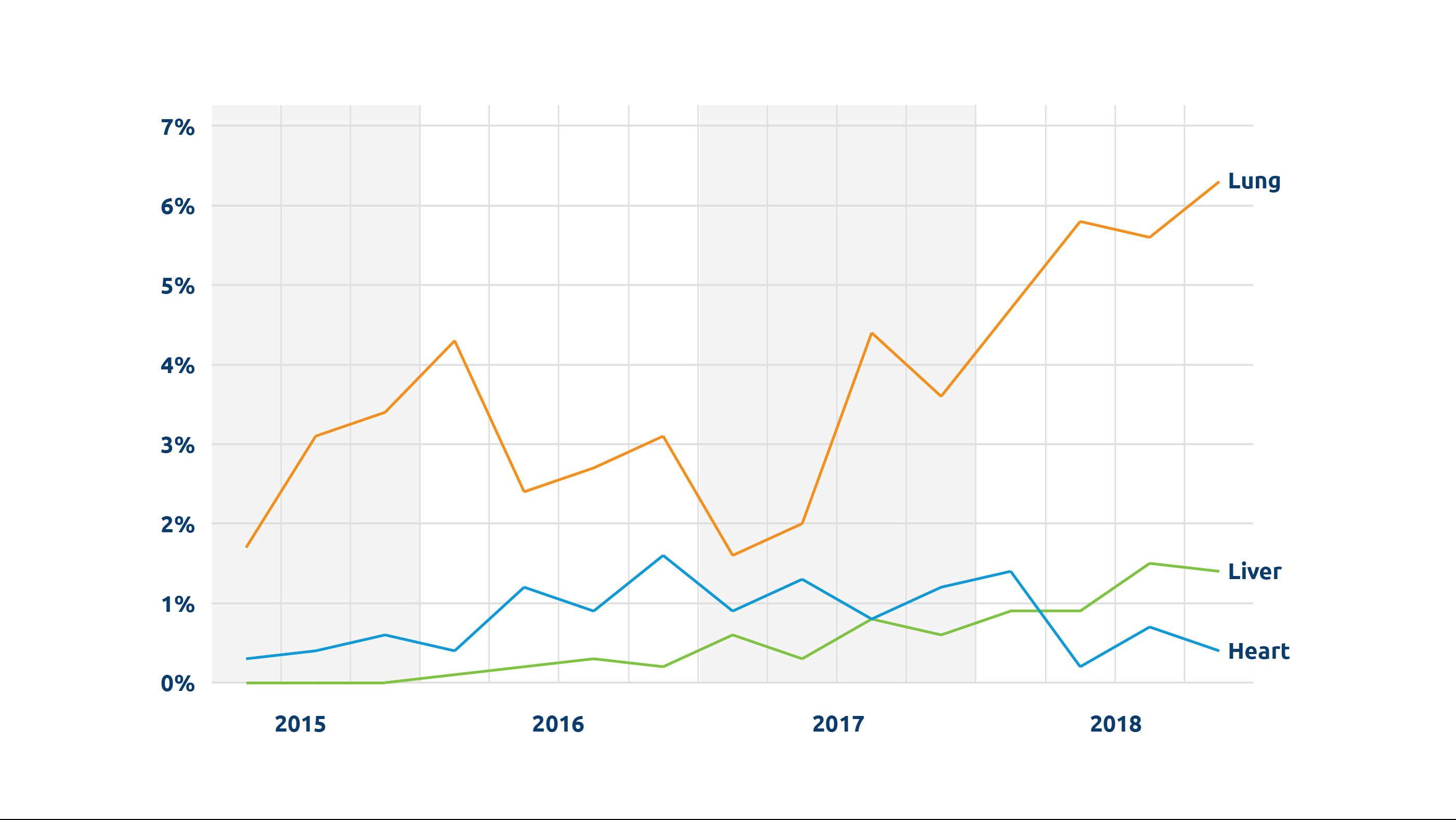
A. Data we have collected at UNOS shows increasing use of the technology, particularly for lungs, but because this technology is still relatively new, most applications have been in the context of clinical trials. Use of the technology is more advanced outside the U.S., particularly in Europe and the UK where much of the early clinical research has been done.
Q. How could this technology potentially affect the future of transplantation in the U.S.?
A. The technology is already being used for DCD heart and lung transplants, and the data so far seems to show outcomes comparable with transplants using standard criteria organs. This is a completely new source of organs, so already we can see the potential that this technology will help increase the number of organs available for transplant.
Q. What other potential benefits could the technology offer?
A. Whether this technology will ultimately benefit patient outcomes and survival has not yet been determined. However, it is easy to foresee the wide range of potential. Extending organ preservation time could expand allocation. Ex vivo perfusion could abrogate the problem of ischemia reperfusion injury or allow the organ to recover from it, and it could possibly be used actually to improve organ function—whether by treating infections or even by changing immunogenicity. It is possible that implementing this technology could reduce overall transplant costs by shortening pre- and post-transplant hospitalization time.
Q. What are the most significant challenges to adopting this technology?
A. Although the promise and potential of this technology are widely appreciated within the transplant community, there are many logistical questions still to be answered. What is the best approach to implementing this technology? Who pays for it, who owns it, who operates the machinery, what training will be required to use it? Who is in charge of the perfusion and when does it occur—at the time of procurement, at a free-standing perfusion center, at the recipient transplant hospital? Or, if the machines are portable, how do you transport them from place to place? In addition, we can’t yet assess whether the benefits will be greater than the costs and challenges of widely adopting this technology.