Thanks to the HIV Organ Policy Equity Act (the HOPE Act), 100 organ transplants have been performed for HIV-positive candidates willing to accept organ offers from HIV-positive donors. As of December 18, 15 hospitals participating in HOPE Act protocols performed those 100 transplants. These include 69 kidney transplants and 31 liver transplants, involving organs from 49 deceased donors.
“The collective effort by the transplant community is bringing more opportunity to these patients. As a result, it also expands access for everyone waiting for an organ transplant,” said UNOS Chief Medical Officer David Klassen.
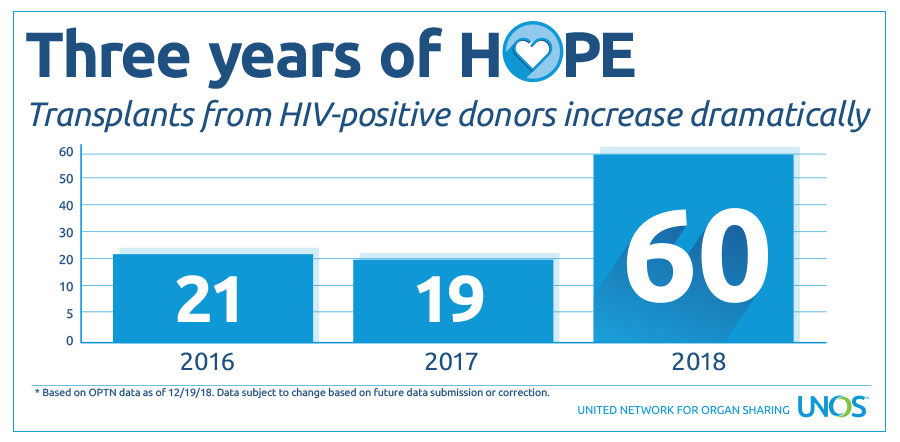
Most of the transplants allocated through the HOPE Act have occurred in 2018, as more and more organ procurement organizations have developed recovery protocols. Organs from donors that initially test positive for HIV have been transplanted into HIV-positive recipients since 2016; 19 in 2016, 21 in 2017 and 60 so far in 2018. This indicates that more and more HIV-positive people are becoming aware that they can leave the legacy of life through organ donation.
Supporting HIV-positive candidates
UNOS has been supporting HIV-positive candidates through the HOPE Act since its implementation. “The HOPE act has provided the ability to transplant organs from individuals not previously considered as donors. This has increased the opportunity for HIV+ recipients on the waiting lists to be transplanted,” said Klassen. “The HOPE Act program was slow to get started but in recent months as more transplant centers have initiated HOPE Act transplant programs and OPOs have identified additional donors, the number of transplants has increased substantially.” Signed into law November 2013 and implemented November 2015, the HOPE Act opened the door for HIV-positive candidates to receive and donate organs. The act allows research on transplantation of organs from donors identified as HIV-positive into HIV-positive candidates under approved research protocols. Organ procurement organizations can run matches for HIV-positive donors. The only candidates who appear on match runs for these donor offers are those listed at transplant programs that have an IRB-approved protocol, who are confirmed as HIV-positive, and who are willing to accept an HIV positive kidney or liver. Any participating hospital must conduct transplants under IRB-approved research protocols conforming to the Final Human Immunodeficiency Virus (HIV) Organ Policy Equity (HOPE) Act Safeguards and Research Criteria for Transplantation of Organs Infected with HIV, developed by the National Institute of Allergy and Infectious Diseases, one of the National Institutes of Health.
Educating HIV patients about organ donation
Current estimates suggest that more than 1.2 million people are HIV-positive; 35,000 people are newly infected every year. While life expectancy of HIV positive patients nears that of the general population, end-stage liver or kidney disease is expected to increase as the population ages, creating an even greater need for more organs. It’s critically important to educate HIV patients about the HOPE Act and organ donation if the availability of these organs is to grow. Search for a participating transplant hospital.
Bringing hope to the entire transplant community
Transplanting organs from HIV-positive donors into HIV-positive candidates shortens the waitlist, increasing the organ availability from HIV-negative donors for HIV-negative recipients. In addition, it gives hope and comfort to the family of donors, knowing their loved ones have saved the lives of other HIV-positive patients.
