Improvement
Embracing new ideas to increase DCD donation
Impacts from the OPTN DCD Procurement Collaborative
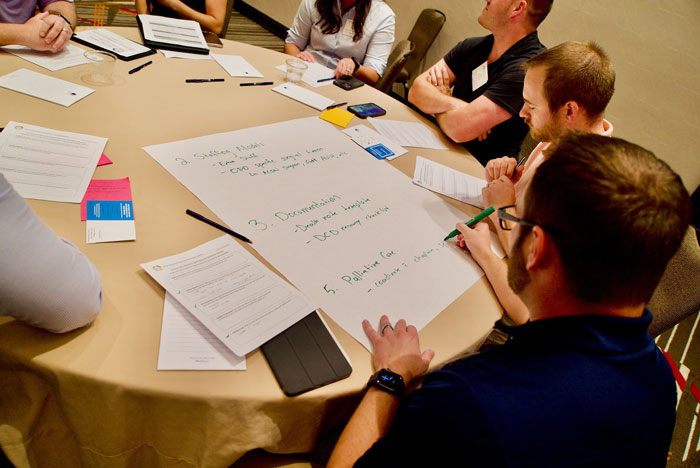
In July of 2022, the Organ Procurement and Transplantation Network (OPTN) concluded a national Collaborative Improvement (CI) project focused on increasing the procurement of organs from donation after circulatory death (DCD) donors. CI initiatives are quality-focused efforts, available at no charge to OPTN members, that are designed to bring organizations and teams together to work on a shared improvement goal. Over the course of two years, more than 75 percent of the nation’s Organ Procurement Organizations (OPOs) participated in one or both of two six-month project cohorts of the OPTN DCD Procurement Collaborative, identifying and sharing effective practices in DCD donor authorization and recovery processes.
“Everybody was willing to share because we all have a common goal of getting people transplanted and caring for the donor family.”
Schawnté Williams-Taylor VP of Family Engagement at LifeGift Organ Donation Center
The OPTN DCD Procurement Collaborative
DCD donors are patients who have experienced severe neurological damage–often as the result of a stroke, head trauma, or suffocation—and are unable to survive without a ventilator. When families choose to discontinue further medical intervention and withdraw ventilator support, end-of-life planning may include organ donation. Over the past decade, research and technological advances have helped make a growing number of lifesaving transplants from DCD donation possible. In 2022, DCD donors represented nearly one third of all deceased donors, thanks in part to the work of the Collaborative. By the time the project concluded, the first cohort had increased DCD donor procurement by 34 percent over all of 2021, and the second cohort by 28 percent over the comparable six-month period in 2021.
One year later, three participants from the Collaborative offered their perspectives on the benefits of the collaborative learning process and the day-and-a-half Learning Congress at the conclusion, as well as on the longer-term impact on their own organization’s practices.

Nearly 33%
In 2022, DCD donors represented nearly one third of all deceased donors, thanks in part to the work of the Collaborative.
Hearing “how other OPOs were moving forward with DCD first-person authorization was instrumental with our team, so we could find strategies of how to implement that.”
Javier Nieto, Senior Manager, LifeGift Organ Donation Center
Sharing for a common goal
Rodney Pilson, Manager of Approach and Referral Optimization for HonorBridge, in North Carolina, said that one of the most valuable aspects of the collaborative was not any one specific takeaway but rather the broader commitment to a common goal and to sharing insights and ideas to help reach that goal.
“The collaborative was rich in this idea that ‘we’re all in this together,’” he said. “I loved just hearing and letting people know that it’s OK to reach out. You don’t have to figure it out by yourself as a department or organization; we’re really in this together the to move the needle.”
The exchange of ideas and practices was also a vital part of the experience, he stressed. “Not only did the collaborative highlight a lot of the industry’s best practices around DCD processes, but it also highlighted how the decisions and the projects that were being shared were actually built upon or inspired by other projects going on at other OPOs,” he said.
“Everybody was willing to share,” agreed Schawnté Williams-Taylor, Vice President of Family Engagement and Donation Services for the OPO LifeGift in Texas, “because we all have a common goal of getting people transplanted and caring for the donor family.”

It’s OK to reach out
“The collaborative was rich in this idea that we’re all in this together.”
“We increased our authorization rate with non-registered African American donor families from historically 30 percent or lower to 56 percent.”
Rodney Pilson, Manager of Family Services, HonorBridge
Improving communications
The participants also highlighted two key takeaways from the Collaborative, both of which involved communication between hospital staff, OPO staff and donor families. The first of these was working with hospital staff to plan for timely notification from the hospital to the OPOs when families appear to be nearing readiness for end-of-life decisions.
Williams-Taylor noted that too often she has heard families say, “I wish you had been here two days ago.” Helping hospital staff to identify “soft cues” that might indicate family readiness in turn makes it possible for OPOs to be prepared if the family expresses interest in end-of-life planning that could include organ donation, and ensures that the OPO “is able to provide information when the family is ready,” she said.
Since the Collaborative, Pilson’s OPO has developed a protocol with referring hospitals to answer just two questions that can help begin the process of evaluating a family’s readiness. The first question asks whether a family is indicating that they are prepared to accept the poor prognosis for a loved one on life support. The second asks whether the family seems ready to choose comfort care within the next day or two.
If either question is answered with a “yes,” in conjunction with hospital staff, “that activates a family readiness assessment to happen,” said Pilson.

Two questions to evaluate readiness
- Is the family indicating that they are prepared to accept the poor prognosis for a loved one on life support?
- Does the family seems ready to choose comfort care within the next day or two?
Affirming a donor’s decision
The other important takeaway from the Collaborative was the benefit of developing consistent, shared messaging with referring hospitals on talking with families about first-person authorization when a patient is determined to have previously registered as a donor.
Javier Nieto, Williams-Taylor’s colleague and an abdominal organ clinical recovery surgeon with LifeGift, said that hearing “how other OPOs were moving forward with DCD first-person authorization was instrumental with our team, so we could find strategies of how to implement that.”
“Our goal,” added Williams-Taylor “is to empower a family to support their loved one’s decision.”
At HonorBridge, Pilson said, the Collaborative provided ideas about “having a different type of conversation with the hospital” regarding first-person authorization, to assure that both hospital and OPO staff are providing a clear message to the family that the decision to be a donor was already made by the patient. “Coming back and implementing those ideas, we found ourselves having much more effective conversations with our families. When everyone’s consistent in honoring a decision, now we can provide a clear message to the family.” The result, he said, is that HonorBridge has increased DCD authorization from 78 to 95 percent. Additionally, as a result of this work, “We increased our authorization rate with non-registered African American donor families from historically 30 percent or lower to 56 percent.”

The focus
Each of the two OPO cohorts worked collaboratively for a six-month engagement period on improvement efforts in these key areas:
- Optimizing clinical practices and staffing structures
- Strengthening donor hospital and transplant program relationships
- Enhancing the process for obtaining authorizations
Read more
Collaboratives continue
- Summer 2022: The OPTN DCD Procurement Collaborative wrapped up
- July 2023: The eight-month OPTN DCD Lung Transplant Collaborative concluded
- 29 adult lung programs participated
- A Learning Congress, which all adult lung programs were invited to attend, was held in September of 2023
- July 2023: The six-month OPTN Offer Acceptance Collaborative also concluded
- More than 80 transplant programs from around the country participated
CI initiatives are quality-focused efforts, available at no charge to OPTN members, that are designed to bring organizations and teams together to work on a shared improvement goal.